Division of Gynecological Oncology
The Division of Gynecologic Oncology at the NCT is responsible for diagnostics and therapy of breast cancer in women and men, and abdominal cancer in women in all stages of the disease. Through a comprehensive clinical study program, patients also have access to new procedures prior to certification. Supplementary translational programs accelerate the transferal of new knowledge from basic research. The aim is to provide optimal personalized treatment for each individual patient according to their condition.
Therapeutic Structures of Gynecologic Oncology
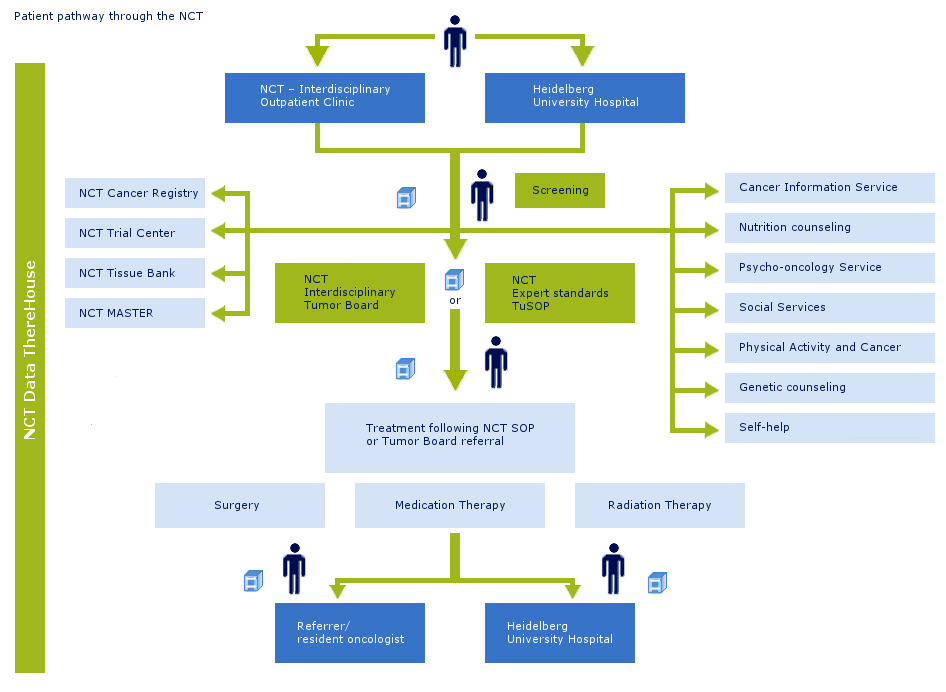
The interdisciplinary tumor outpatient clinic (Tumorambulanz) offers a sophisticated advisory service and is the primary point of contact for oncological patients and their families. Previously obtained results are considered and evaluated before a treatment plan is created. In the outpatient clinic, all approved system therapies are administered on an ambulatory basis.
Inpatient services are available for diagnostic procedures and therapeutic measures that call for the patient’s admission. Some of these patients are admitted to the Hospital for Internal Medicine ("Medizinische Klinik"), Women's Hospital ("Frauenklinik"), Department of Radiology ("Strahlenklinik") or the Department of Surgery ("Chirurgische Klinik"). The NCT works in close clinical cooperation with the Salem Hospital, as well as the Vinzentius Hospital in Heidelberg, and the Kreiskrankenhaus Heppenheim.
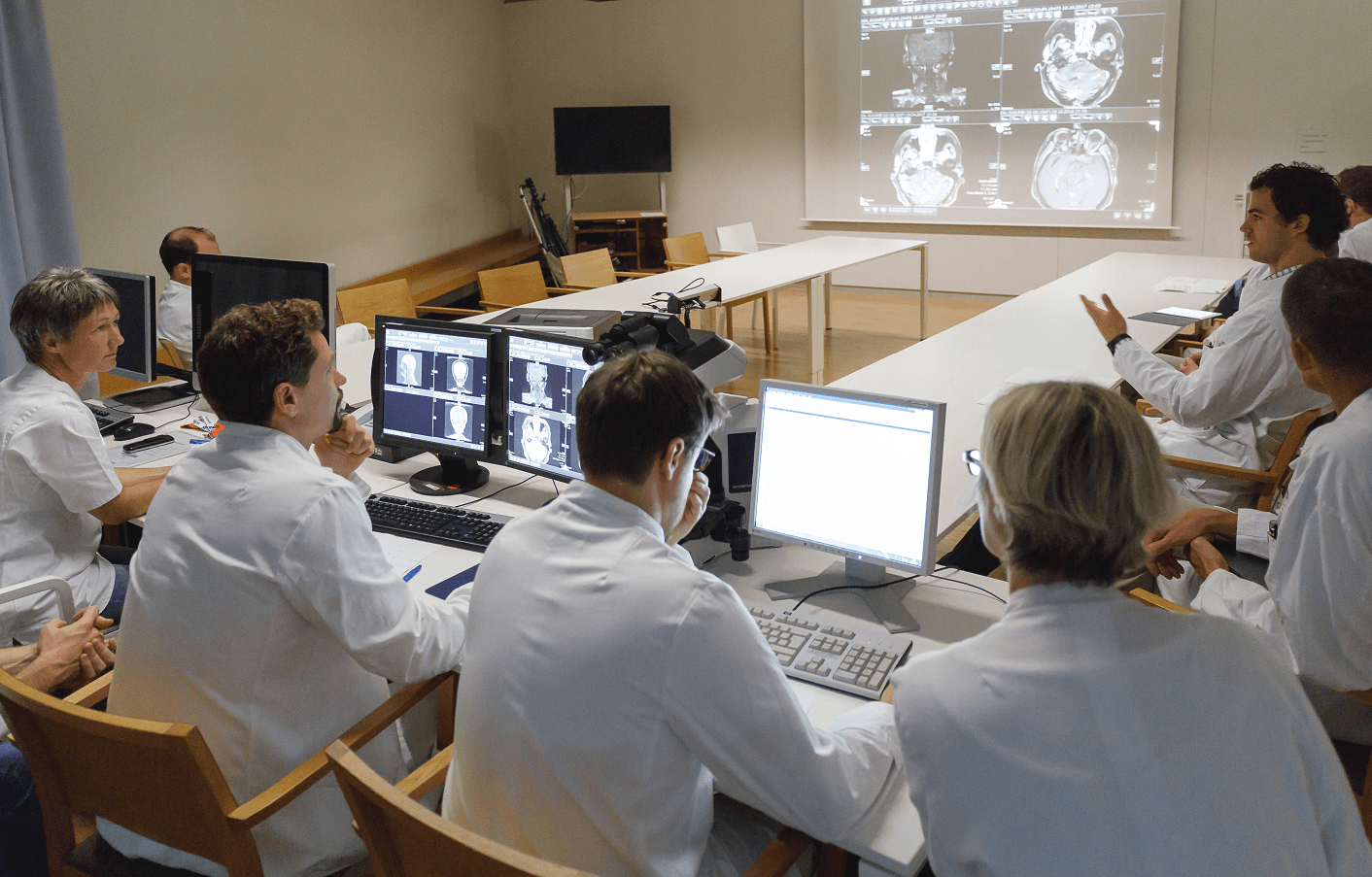
Interdisciplinary Tumorboard
In the interdisciplinary Tumorboards, medical histories are viewed including all relevant diagnostic findings– if necessary including original documents. These are evaluated, discussed and a procedure is then determined. These Tumorboards consist of representatives of all disciplines relevant to diagnostics and therapy. The basis for the discussion are the illness-specific Standard Operating Procedures (SOPs) of the NCT, which are consensus-based and updated annually. This procedure requires a close collaboration of all disciplines involved, but it guarantees optimal patient care.
Standardized treatment paths
The specialists from every cancer program identify specific procedures, so called Standard Operating Procedures, SOP for each cancer, which are used for treatment of all patients diagnosed and treated at the NCT. Therapeutic concepts are established in individual interdisciplinary tumor conferences for patients that do not fit into this framework of SOPs due to emergence of a second tumor, having exhausted the current standard therapy, or because they are in a relapse situation.
As a rule, the referring physician is always informed about any recommendations. Wherever appropriate, patients are encouraged to take part in clinical studies. If medicative therapy such as chemotherapy or immunotherapy is necessary, this can very often be administered in the outpatient clinic. The application takes place in the day care units (Tagesklinik I and II). The day care units are open Monday to Friday between 8 am and 4 pm.
Research
Together with the other NCT units, the research spectrum of the Gynecological Oncology Division has the aim to translate state-of-the-art-basic research into clinical application as fast as possible.
We are working to offer patients new and more innovative tumor therapies in the future. The research groups therefore have a common goal: Based on identifying new, molecular target structures and tumor-specific immunological mechanisms involved in carcinogenesis, they are aiming to develop therapies for prevention and delay of disease progression.
Basic research at the Gynecological Oncology Division in cooperation with working groups at the DKFZ and external partners have the following objectives:
- Identification of novel target genes in breast cancer patients and development of sequencing based prognostic and predictive profiles and their transfer into clinics (Lichter/Zapatka/Schneeweiss).
- Characterization and functional analysis of metastasis –initiating stem cells in breast and ovarian cancer (Trumpp/Baccelli/Sprick/Schneeweiss).
- Evaluation of mutation and methylation signatures, microRNAs and metabolites in peripheral blood as early detection and prognostic markers in breast cancer (Burwinkel/Schneeweiss).
- Analysis of genome-wide transcriptional programs regulating invasive growth of human breast and brain cancer (Wiemann/Yarden/Schneeweiss).
- Validation of aCGH BRCAnes classifiers as predictors for response to akylating agents, platinum salts and PARP-inhibitors (Marmé/Linn/Altevogt).
- Evaluation of the prognostic value and biologic impact of exosomes in breast and ovarian cancer (Marmé/Altevogt).
- Evaluation of the prognostic and predictive value of FGF receptors, in particular FGFR4, and their ligands in breast and ovarian cancer (Kommoss/Marmé).
- Detection of new epigenetic marker for radiotoxicity after intraoperative radiotherapy in breast cancer (Chang-Claude/Rössler/Schneeweiss).
- Evaluation of the impact of menopausal hormone therapy, life style and genetic factors on cancer incidence and cancer mortality (Chang Claude/Rössler/Schneeweiss).
- Functional characterization of the breast cancer antigen NY-BR-1 and its clinical significance as a target protein for immunotherapeutic approaches (Zörnig/Jäger/Schneeweiss).
- Identification of NY-BR-1 specific T cell epitopes and establishment of TCR transduced T cell clones for adoptive T cell transfer strategies (Zörnig/Jäger/Eichmüller/Schneeweiss).
- Molecular classification of breast cancer, determination of breast cancer proliferation and quantification of immune cell composition by RT-qPCR from fixed and fresh frozen biopsies to predict response and prognosis after neoadjuvant chemotherapy (Wirtz/Sinn/Marmé/Schneeweiss).