Every year, NCT Heidelberg project teams can apply for funding from the "Donations against Cancer" program. A selection committee of experts from various disciplines assesses the applications submitted. After examination, research projects are selected to be funded with donations. 2025, the selection committee has chosen four projects from the field of translational research and three projects from the field of nursing care and counseling:
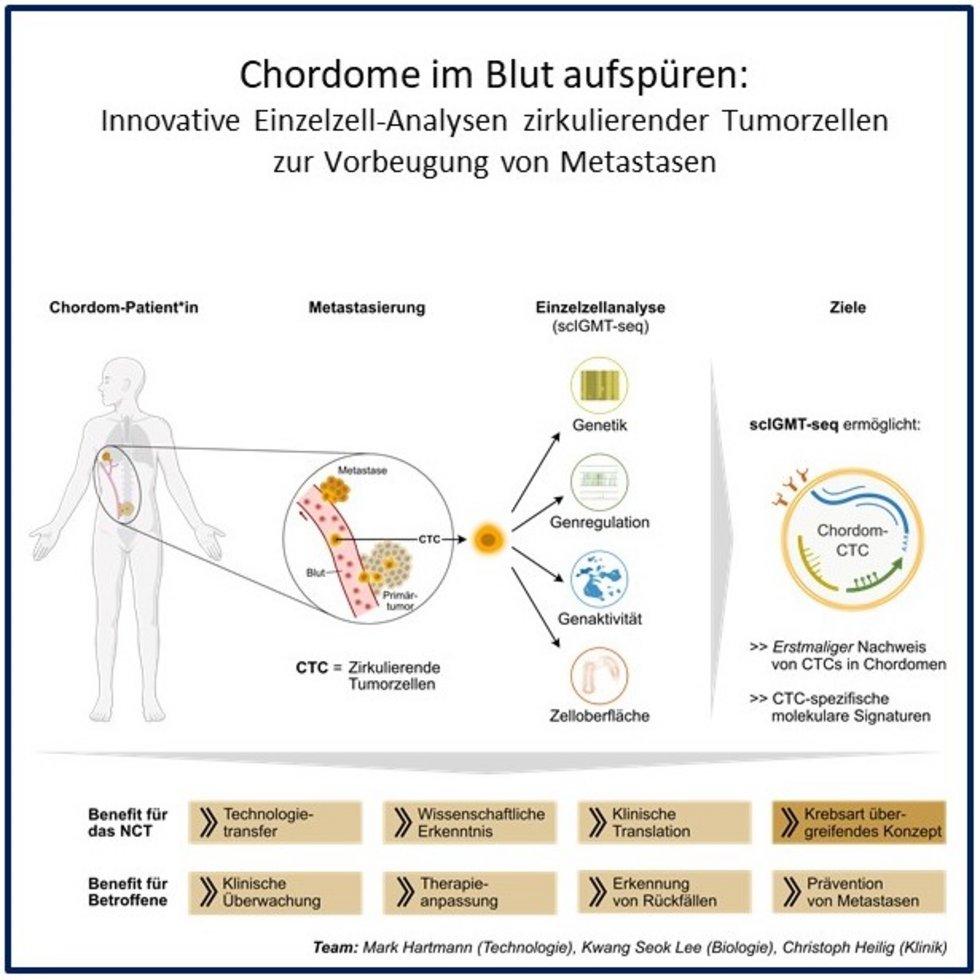
Tracing Chordomas in the Blood: Innovative Single-Cell Analyses of Circulation Tumor Cells to Prevent Metastasis
Dr. Mark Hartmann, Dr. Kwang Seok Lee, Dr. Christoph Heilig
Chordomas are rare, slow-growing but aggressive tumors of the spine and skull base; chordomas often recur and can metastasize. Circulating tumor cells (CTCs) in the blood are of central importance for the development of metastases. However, CTCs have not yet been studied in chordomas.
The project uses a new single-cell technology (scIGMT-seq) that simultaneously analyzes the surface profile (immunotype), genetic (genotype) and epigenetic changes (DNA methylation), and gene activities (transcriptome) of individual cells. The aim is to reliably detect CTCs for the first time and characterize them in detail at the molecular level. In blood samples from patients with advanced disease, potential tumor cells will be identified, collected, and further analyzed using flow cytometry. Flow cytometry detects individual cells in a liquid suspension using a laser beam.
As a proof of concept, the project aims to provide markers for clinical monitoring, therapy adjustment, and earlier relapse detection, thus laying the foundation for further studies and new therapeutic approaches to chordomas. In the long term, this could lead to new treatment options for preventing metastases.
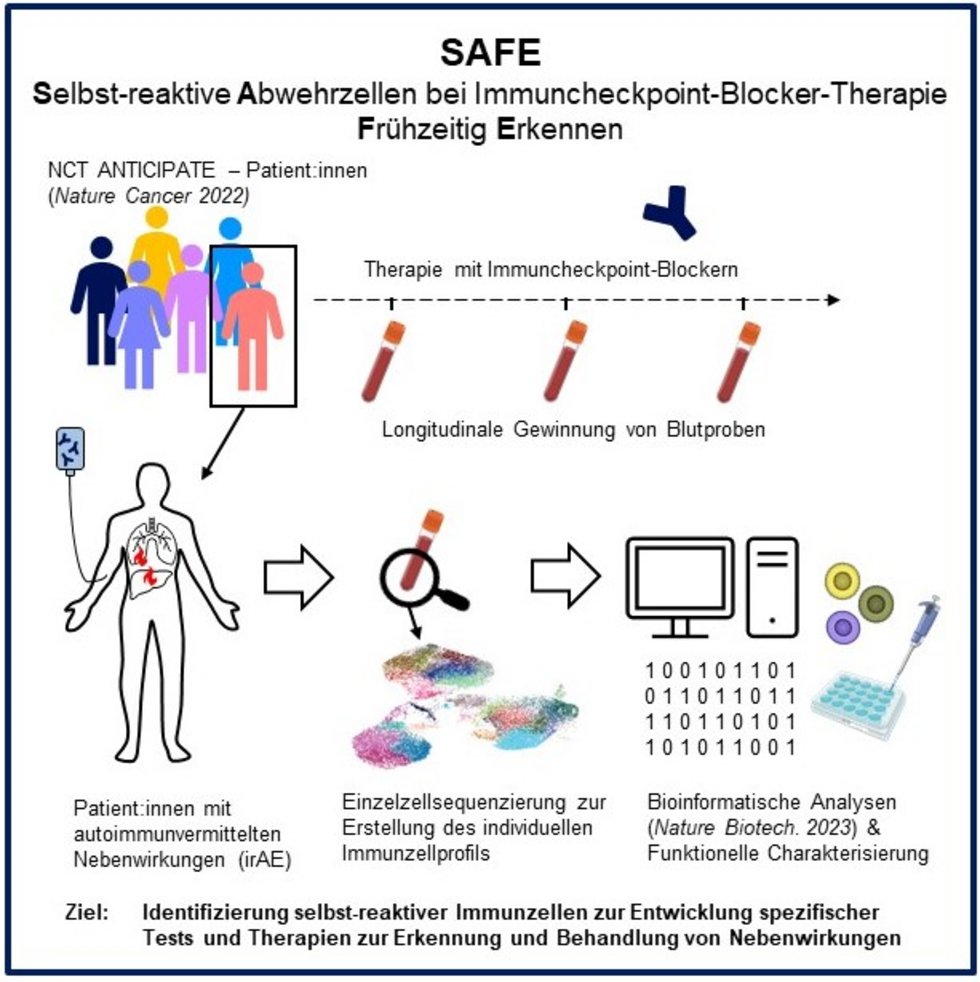
SAFE – Single Cell Analysis of Self-reactive T cells in Immune Checkpoint Therapy
Joscha Kraske, Dr. Thomas Walle
Immunotherapy with immune checkpoint inhibitors has significantly improved the treatment of many types of cancer. However, it can also cause activated immune cells to attack healthy organs such as the liver, lungs, or intestines. Specific “self-reactive” immune cells are thought to be responsible for this. However, it is not yet known how they differ from tumor-reactive immune cells.
The project uses single-cell sequencing to examine immune cells in the blood of patients receiving immune checkpoint inhibitor therapy. The activity of thousands of cells is read out for each individual patient in order to identify cell groups associated with immune-mediated side effects using modern bioinformatic methods. The function of the identified cells is then examined in more detail in the laboratory. This new biological data is linked individually with clinical data. The aim is to identify patients at increased risk of immune-mediated side effects at an early stage through the development of diagnostic tests and to lay the foundation for new therapies that specifically treat side effects without compromising the success of the therapy.
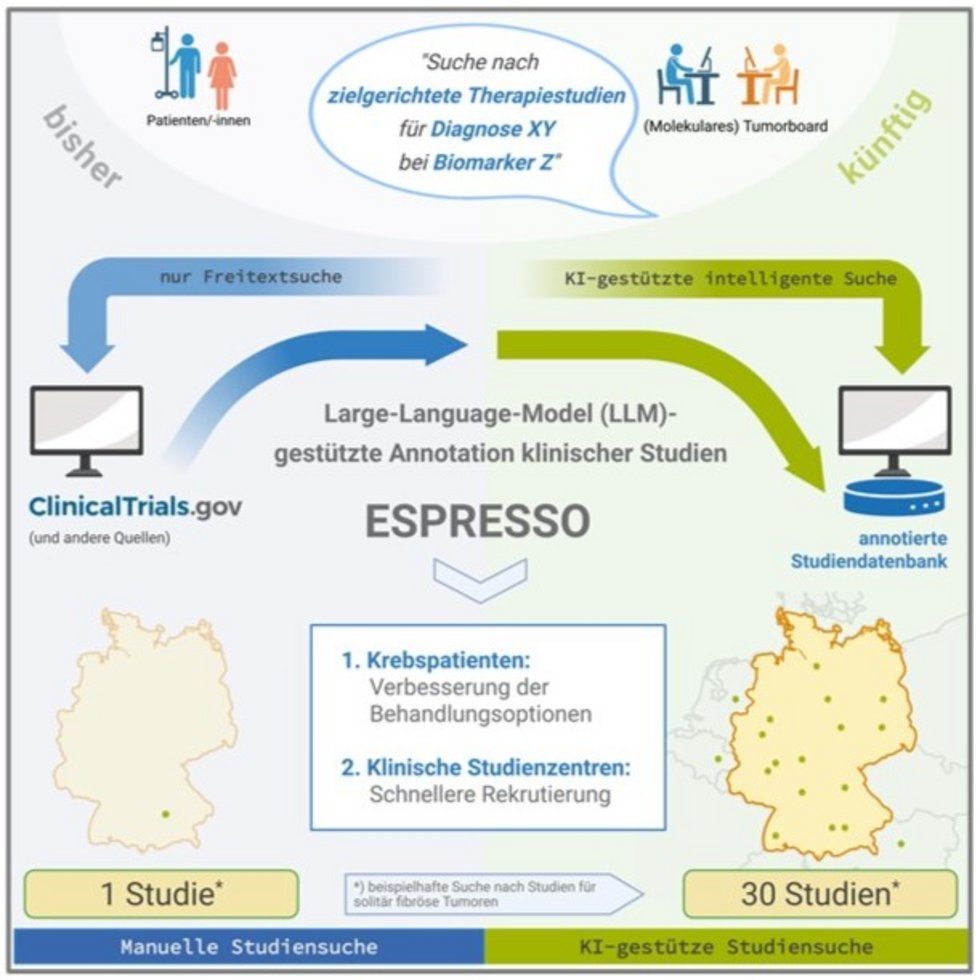
ESPRESSO = Eligibility Screening of clinical trial Protocols using Retrieval-Enhanced Semantic Searches and Ontologies
Dr. Simon Kreutzfeldt, Dr. Eva Krieghoff-Hennig, Eva Reisinger, Nils Hammer
Clinical trials enable cancer patients to access innovative therapies that go beyond the standard of care. This is particularly relevant for rare tumors, for which there are often few effective treatments. However, finding suitable trials is difficult: inconsistent protocols and inconsistent terminology for cancer types, drugs, and biomarkers lead to incomplete results.
ESPRESSO addresses this problem with an automated, AI-supported annotation method. It analyzes study protocols from study databases, structures and harmonizes information on treatment arms, cancer types, biomarkers, and therapies, and supplements missing data from other publicly available sources. In a pilot study, 30 suitable studies were identified for a patient with a rare tumor disease – conventionally, only one study was found.
The user-friendly database, which is updated daily, is accessible via a web interface and an API interface and can be integrated directly into tumor board software. Thanks to its high degree of automation, the platform enables fast, comprehensive searches for studies on an ongoing basis, improves patient care, and supports recruitment for clinical study centers in the One NCT.
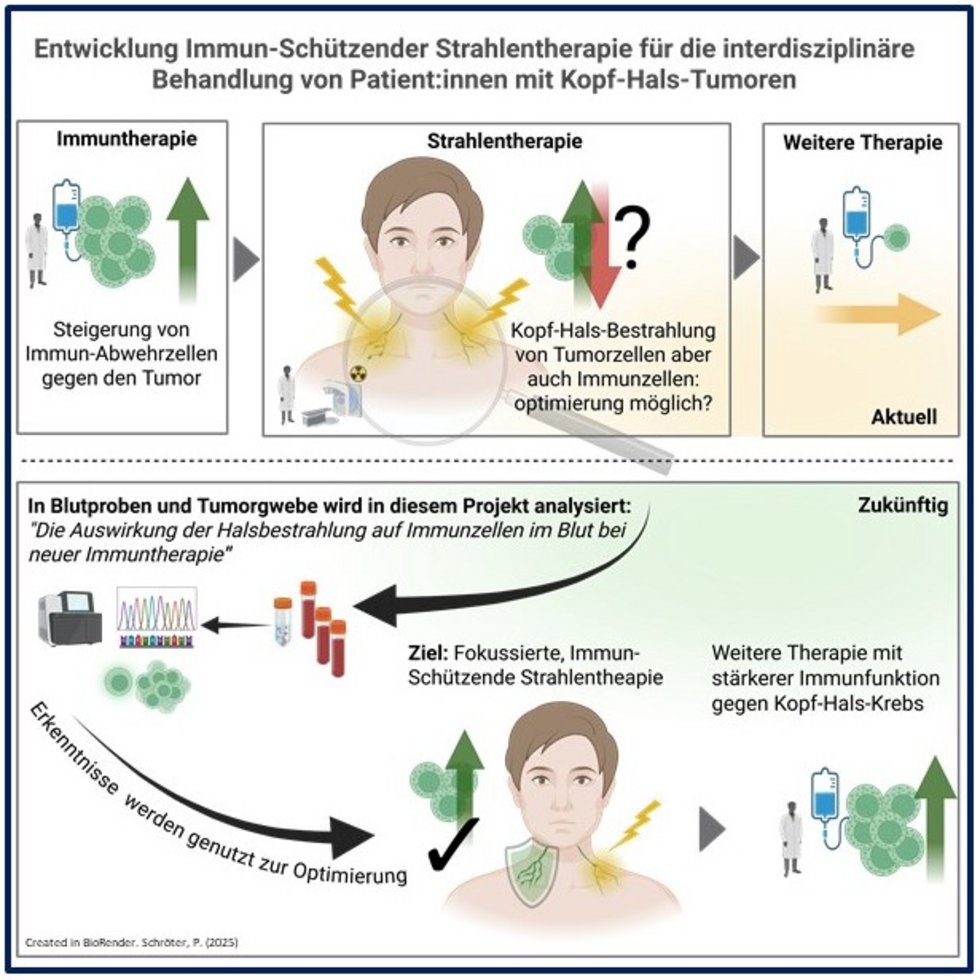
Targeting Tumor Cells – Preserving Immune Cells: Developing Immuno-Compatible Radiotherapy to Advance Interdisciplinary Treatment Strategies for Patients with Head and Neck Cancer
Dr. Philipp Schröter, Dr. Florian Stritzke, PD Dr. Thomas Held, PD Dr. Tilmann Bochtler
New studies show that immunotherapy can be combined with surgery and radio(chemo)therapy in advanced head and neck cancer. While immunotherapy strengthens immune cells in the fight against tumor cells, radiation can weaken the immune system.
Until now, extensive prophylactic neck radiation after surgery has been the standard treatment for removing the smallest tumor remnants. However, it also affects many immune cells and lymphatic vessels, and its effects on the immune system have not yet been sufficiently studied. A precise understanding of the effects of radiation on the immune system is therefore necessary in order to optimize the therapy.
In the pilot project, patients with operable head and neck cancer are accompanied through all stages of therapy, and a “fingerprint” of the immune cells important for tumor defense is created from tumor, lymph node, and blood samples using T-cell receptor sequencing. This allows the identification of immune responses that arise during immunotherapy, decline during radiation therapy, or circulate in the blood afterwards.
The goal is more targeted radiation therapy that spares immune cells, strengthens sustained immune responses, and, in combination with immunotherapy, better combats head and neck cancer.
SDM Competent: Shared Decision Making and Patient-Centered Communication Skills in Oncology
Prof. Dr. Christiane Bieber, Dr. Cindy Körner
Today, numerous treatment options are available in oncology, such as immunotherapy, targeted therapies, chemotherapy, surgery, and radiation. Treatment decisions are complex and involve different risks and benefits. For years, guidelines have recommended shared decision making (SDM) between patients and physicians in order to take individual wishes, life circumstances, and values into account.
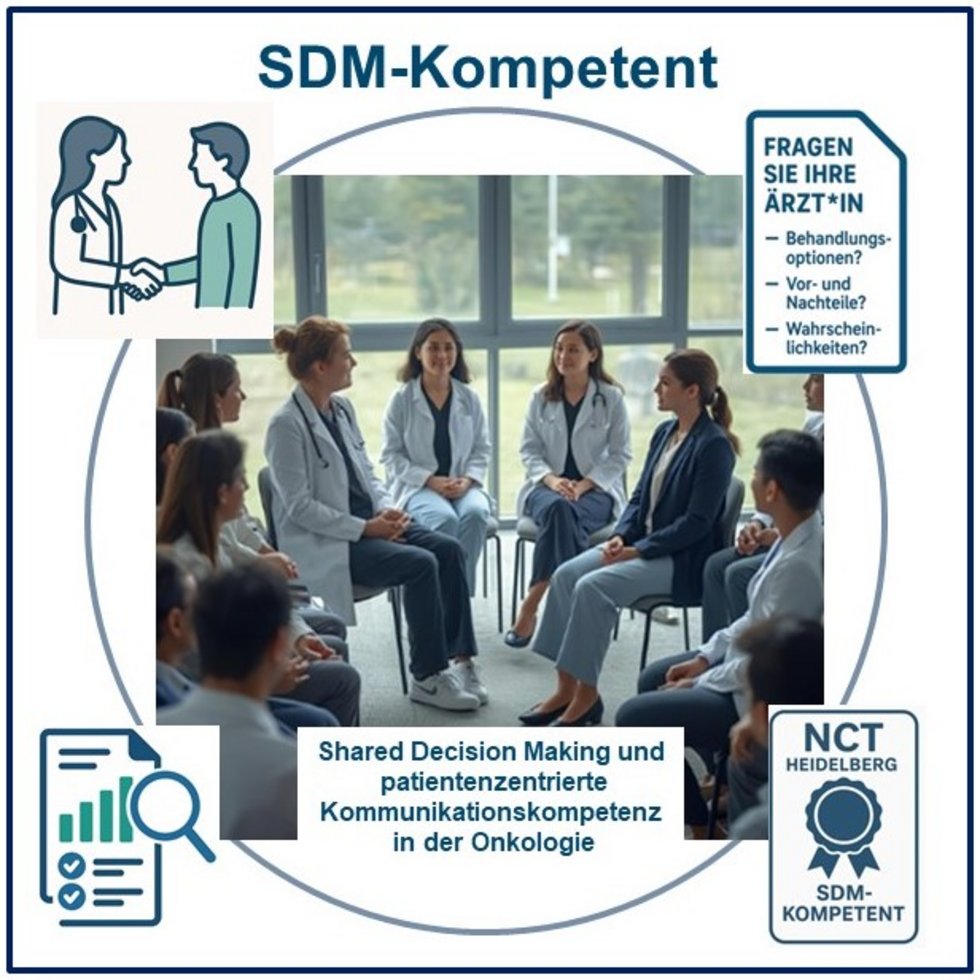
However, SDM is still rarely used in everyday clinical practice, at least in the experience of patients. Many physicians are open to the idea, but without specific training, implementation is rarely successful. Specific communication skills are crucial, such as actively incorporating the patient's perspective, dealing with uncertainties, weighing risks and benefits, and handling emotionally stressful situations.
The project aims to teach SDM skills to oncologists through communication training, including patient input, knowledge transfer, group discussions, reflection tasks, example videos, role-playing, video feedback, and practical exercises. The concept is based on approaches developed and tested with the patient advisory board at the NCT Heidelberg.
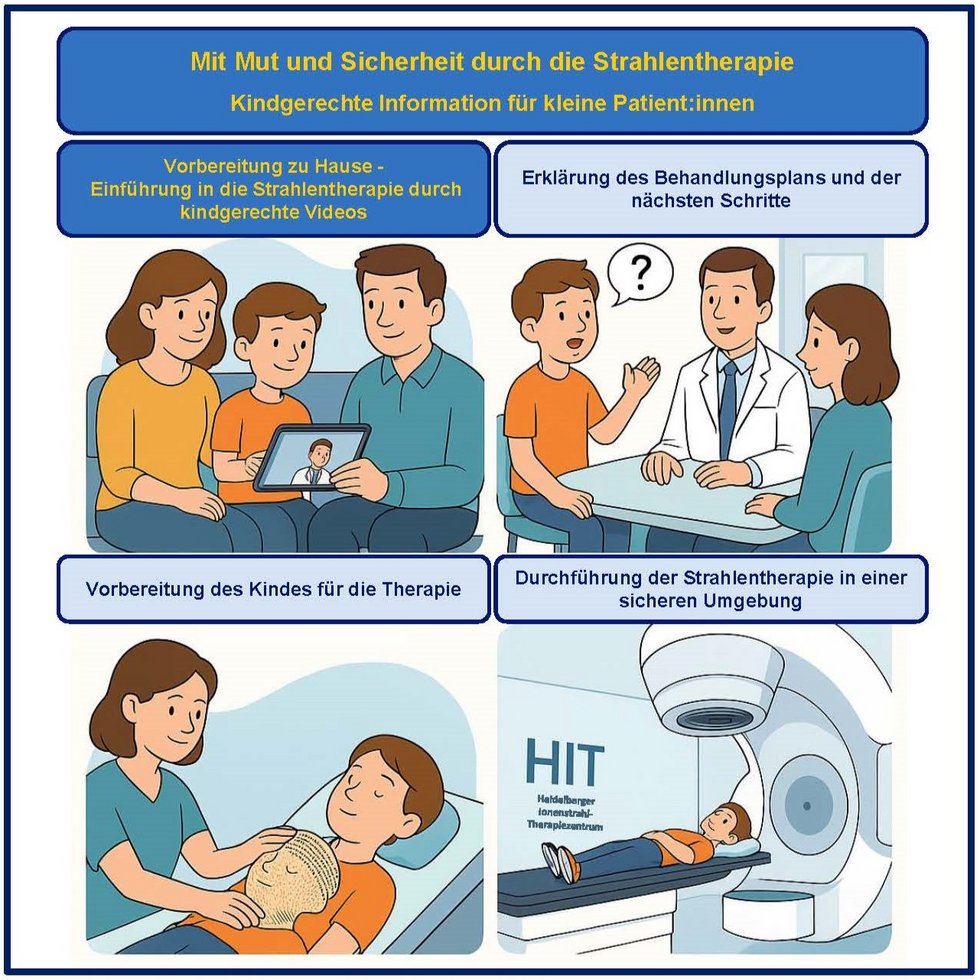
Facing Radiotherapy with Courage and Confidence: Child-friendly Information for Young Patients
PD Dr. Semi Harrabi, Dr. Maximilian Deng
Radiation therapy can be particularly frightening for children: unfamiliar equipment, large rooms, unknown procedures, and the need to lie still often lead to anxiety and overwhelm. This often makes anesthesia necessary.
At the Heidelberg Ion Therapy Center (HIT), child-friendly informational videos are being created in collaboration with child psychologists and parent representatives. They explain the treatment process step by step—from the initial consultation to the planning CT scan and the creation of the individual mask to the radiation treatment at HIT. Clear language, vivid images, animations, and real footage provide children with guidance and reassurance.
The videos build trust, encourage children, and show that a team of doctors, nurses, physicists, and therapists is there to support them. Parents can watch the films together with their children to better understand the steps involved in the therapy. The project helps to reduce fears, lower the number of anesthesias, facilitate the treatment process, and provide lasting guidance for children and families.
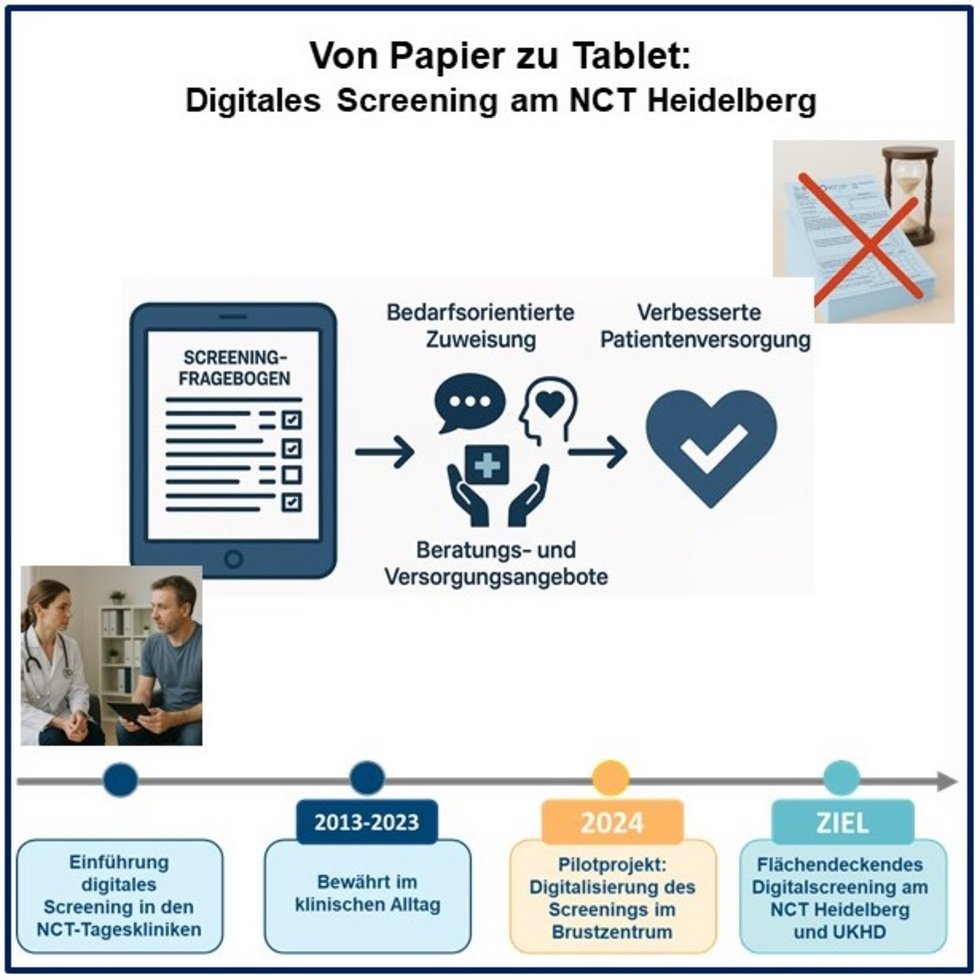
From Paper to Tablet: Broad Implementation of a Digital Distress Screening at NCT Heidelberg
Dr. Till Johannes Bugaj, Dr. Miriam Grapp, Anne-Kathrin Müller
International professional associations recommend distress screening, a standardized procedure for assessing stress such as anxiety, depression, social concerns, or physical symptoms, as an integral part of oncological care. It enables patients to be referred to appropriate support services at an early stage. In practice, screening is often paper-based. As a result, results do not always reach the treatment teams quickly and can easily be overlooked.
In 2013, the NCT Heidelberg introduced a digital screening system that serves as a model for the rest of Germany. Until now, its use has been limited to the NCT building. In 2024, a successful pilot project with tablet-based screening was launched at the Breast Center. Expansion to other organ centers is therefore feasible.
The aim of the project is to introduce digital screening in all organ centers. Results are immediately available to the treatment teams in digital form, so that patients with a high need for support can be referred to psycho-oncology, social services, nutritional counseling, exercise, and other services. At the same time, a valuable database is created for research, quality assurance, and future innovations.