Press release from Heidelberg University Hospital (UKHD)
Researchers at Heidelberg University Hospital and the German Cancer Research Center have identified a genetic signature that is typical of certain glioblastoma tumor cells. These particularly aggressive nerve cells network with each other and give brain tumors their enormous resistance to therapies. Thanks to the gene signature, the effect of new therapies can be better tested in future. It also reveals previously unknown, possible weak points of the tumor cells. The work has recently been published in Nature Communications.
A special characteristic of its tumor cells makes glioblastomas incurable to date: they swarm out, network and permeate the brain with a network of wafer-thin cell connections. These "supply routes" keep the brain tumor alive even after most of it has been surgically removed and the rest irradiated and treated with medication. Now, for the first time, researchers from the Heidelberg Medical Faculty at Heidelberg University and the German Cancer Research Center (DKFZ) have created a genetic profile that enables them to clearly distinguish the "network cells" from other cells in the tumor. The signature consists of 71 genes, certain sections of the genome that are read significantly more frequently in the tumor cells as soon as and as long as these cells network. This knowledge opens the door to much more targeted research into urgently needed new therapies.
"The genetic profile for cross-linked tumor cells is a decisive step forward, both for the understanding and further research of this aggressive type of cancer, as well as for possible future therapies," says Professor Dr. Wolfgang Wick, Medical Director of the Department of Neurology at Heidelberg University Hospital (UKHD) and Head of the Clinical Cooperation Unit "Neurooncology" of UKHD and DKFZ as well as spokesperson of the Collaborative Research Center 1389 "UNITE GLIOBLASTOMA - Overcoming the Therapeutic Resistance of Glioblastomas", in which the now published work was developed. "An important goal of new therapies is to disrupt or prevent the cross-linking of glioblastoma cells. With the gene signature, we can now reliably check for the first time whether drugs are effective in patients."
Snapshot of the binding status of the glioblastoma cells
The scientists benefit from the fact that the characteristic signature is much stronger when the tumor cells are actually interconnected. When they removed the connections between living glioblastoma cells in the experiment, their genetic activity also changed and the signature was significantly reduced. "We assume that the gene signature represents a snapshot of the binding status of the glioblastoma cells at the time of sampling," explains Dr. Tobias Kessler, senior physician at the Department of Neurology at the UKHD and Heidelberg Medical Faculty. "It can therefore provide information on whether a drug that we administer before the operation or the removal of a tissue sample influences the ability to cross-link."
The new findings have already led to a Germany-wide study being conducted by the UKHD and the National Center for Tumor Diseases (NCT) in Heidelberg: up to 66 patients with recurrent glioblastoma are given either a specific epilepsy drug, which could potentially hinder the tumor cells from spreading and subsequently networking, or a placebo 30 days before their operation. Whether this approach is successful will become clear after the operation: The removed tumor cells are examined to see whether they have the corresponding gene signature.
Particularly strongly activated gene also indicates aggressive growth in other tumors
A gene contained in the signature could also play a special role in the aggressive growth of glioblastomas and be a suitable target for new therapies: This gene (CHI3L1) with the protein blueprint encoded on it is read particularly frequently in cross-linked glioblastoma cells, correspondingly strongly boosting the formation of the CHI3L1 protein. "We had not previously focused on this gene in glioblastomas, but it marks particularly aggressive growth in other tumor types such as breast, pancreatic and lung cancer," explains first author Dirk Hoffmann from the Clinical Cooperation Unit (KKE) at the DKFZ. The more CHI3L1 protein is produced, the more aggressive the tumors. Studies are currently investigating whether drugs directed against CHI3L1 can slow tumor growth in lung cancer. "If this approach proves successful, it could also be an option for the treatment of glioblastoma," adds Ling Hai, also first author of the study and a member of the KKE team.
The prognosis for patients with glioblastoma is still very poor, despite constantly evolving treatment strategies: even with high-tech surgical procedures, the tumor, which grows into the brain like a network, cannot be completely removed and returns within a year despite combined radiotherapy and chemotherapy. On average, patients survive for less than two years after diagnosis.
Image description
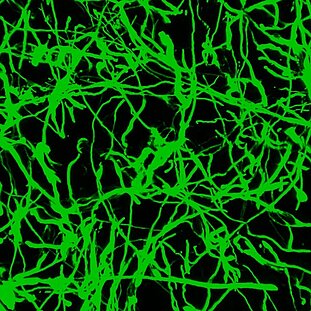
Cross-linked tumor cells from glioblastomas (green) can be distinguished from other cells in the tumor by their gene activity.
The image is available for download here. Use of the image is free of charge, use is only permitted in connection with reporting on the topic of this press release. Use for commercial purposes is prohibited.
Literature
Hai, L., Hoffmann, D.C., Wagener, R.J. et al. A clinically applicable connectivity signature for glioblastoma includes the tumor network driver CHI3L1. Nat Commun 15, 968 (2024).
https://doi.org/10.1038/s41467-024-45067-8. https://www.nature.com/articles/s41467-024-45067-8.
Further information on the Internet
Klinische Kooperationseinheit Neuroonkologie des UKHD und DKFZ
Sonderforschungsbereich “UNITE GLIOBLASTOMA”
Contact
PD Dr. med. Tobias Kessler
Department of Neurology at Heidelberg University Hospital
National Center for Tumor Diseases (NCT)
Medical Faculty Heidelberg of the University of Heidelberg
Phone: 06221 56-7504
E-Mail: tobias.kessler@med.uni-heidelberg.de
You can also find this press release online in our UKHD Newsroom.
Heidelberg University Hospital and Faculty of Medicine: Internationally Renowned Patient Care, Research and Teaching
Heidelberg University Hospital (Universitätsklinikum Heidelberg, UKHD) is one of the largest and most prestigious medical centers in Germany. The Medical Faculty of Heidelberg University (Medizinische Fakultät Heidelberg, MFHD) belongs to the internationally renowned biomedical research institutions in Europe. Both institutions have the common goal of developing new therapies and implementing them rapidly for patients. Heidelberg University Hospital and the Medical Faculty of Heidelberg University employs around 14.500 employees and is committed to providing trainings and qualifications. Every year, around 86,000 patients and more than 1.100.000 outpatient cases are treated in more than 50 clinical departments with almost 2.500 beds.
Together with the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) and the German Cancer Aid, the UKHD established the first National Center for Tumor Diseases (NCT) in Heidelberg. The goal is to provide care at the highest level as an oncology center of excellence and to rapidly transfer promising approaches from cancer research to the hospital. In addition, the UKHD operates in partnership with the DKFZ and the University of Heidelberg the Hopp Children’s Cancer center Heidelberg (KiTZ), a unique and nationally known therapy and research center for oncological and hematological diseases in children and adolescents.
The Heidelberg Curriculum Medicinale (HeiCuMed) is one of the top medical training programs in Germany. Currently, there are about 4.000 future physicians studying in Heidelberg.
Dr. Stefanie Seltmann
Press Officer
Head of Corporate Communications
Phone +49 6221 56-5052
Stefanie.Seltmann@med.uni-heidelberg.de
Julia Bird
Deputy Press Officer
Phone +49 6221 56-7071
Fax +49 6221 56-4544
julia.bird@med.uni-heidelberg.de