In most cases, renal cancer is well responsive to targeted medication; even if there have been occurrences of therapy resistance. However, the choice of the adequate medication is crucial in order to regain control over cancer cells. Scientists of the German Cancer Consortium (DKTK), the National Center for Tumor Diseases (NCT), the German Cancer Research Center (DKFZ) and the Department of Urology at the Heidelberg University Hospital are analyzing in an ongoing clinical trial the mutation patterns of primary tumors and metastases in patients with advanced renal cancer. The identified patterns are meant to support advising each patient, also those with advanced cancer stages, to find an adequate medication for further treatment.
The NCT Heidelberg is a joint institution of the German Cancer Research Center (DKFZ), the University Hospital Heidelberg and the German Cancer Aid.
In Germany 5.530 women and 9.500 men were diagnosed with renal cancer in 2012. Renal cancer is particularly aggressive due to the frequent occurrence of metastases: the kidney belongs to the most blood-supplied organs, which causes proliferating cancer cells to increasingly spread through the blood- and lymphatic vessels.
“Nowadays, metastasized renal cancer is longer controllable in many patients than in the past” explains Holger Sültmann. Sültmann researches the genetic alteration in cancer cells together with his colleagues in the German Cancer Consortium (DKTK) at the National Center for Tumor Diseases (NCT), the German Cancer Research Center (DKFZ) and the Department of Urology at the Heidelberg University Hospital. “Even if resistances occur – which unfortunately is the case with most patients after a certain time – targeted therapeutics can effectively counteract, if the adequate medication is known.”
In the clinical trial MORE (Molecular Renal Cancer Evolution), Sültmann, Carsten Grüllich of the NCT and colleagues from the University Hospital Heidelberg examine which medication could be effective, if the cancer cannot be controlled after a tyrosine kinase inhibitor treatment. In the study, initiated in 2014, the scientists of Heidelberg analyze the molecular alteration in metastasized clear cell carcinoma and the development of resistances occurring in this targeted therapy. “For the first time, we have analyzed the full genetic profile of metastases in patients with advanced renal carcinoma, who have priorly been treated with tyrosine kinase inhibitors and were no longer responsive to the treatment”, as physician and scientist Grüllich reports.
tyrosine kinase inhibitors purposefully intervene into the metabolism of the tumor cell and thereby halt its growth and the spread of metastases.
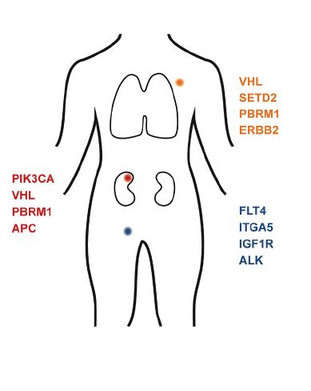
The first results released from the MORE-Study now show that metastases which occur in patients despite treatment cause additional mutations in known cancer genes, as opposed to the original tumor. The BRCA1 or “Breast cancer gene” is one of them among others, which is also involved in the development of ovarian – and prostate cancer. “In some of these cancers, the drug Olaparib has been successfully implemented to prevent cancer cells from DNA repair, causing a programmed cell death” says Stefan Duensing from the Department of Urology at the Heidelberg University Hospital. According to Duensing this approach could also be considered for patients with renal cancer and mutations of the BRCA1 gene.
However, Sültmann acknowledges that the inclusion of the mutation patterns of metastases in the treatment plan of renal cancer would require a confirmation of the results in the form of a larger patient population. Grüllich adds that “next to molecularly targeted therapies we also have to consider other treatment options, such as immunotherapy for example.”
Sültmann sees decisive advantages for patients and the health care in the molecular approach of MORE: “It only takes four weeks from taking the sample to sequencing it and molecular analyses are substantially more cost effective when compared to an unspecified chemo therapy. Furthermore, targeted therapeutics and immunotherapies are subject to fewer side effects. Based on the mutation patterns of metastases we can adjust the second-line therapy individually to the patient in order to gently and effectively eliminate tumor cells.
Dietz S et al. (2017) Patient-specific molecular alterations are associated with metastatic clear renal cell cancer progressing under tyrosine kinase inhibitor therapy. Oncotarget May 23. doi: 10.18632/oncotarget.18200
Press contact:
Dr. Friederike Fellenberg
Nationales Centrum für Tumorerkrankungen (NCT) Heidelberg
Presse- und Öffentlichkeitsarbeit
Im Neuenheimer Feld 460
69120 Heidelberg
Tel.: +49 6221 56-5930
Fax: +49 6221 56-5350
E-Mail: friederike.fellenberg@nct-heidelberg.de
www.nct-heidelberg.de
Dr. Alexandra Moosmann
Presse- und Öffentlichkeitsarbeit
Deutsches Konsortium für Translationale Krebsforschung Deutsches Krebsforschungszentrum
Im Neuenheimer Feld 280
69120 Heidelberg
Phone: +49 6221 42 1662
Email: a.moosmann@dkfz-heidelberg.de
www.dktk.org
Dr. Sybille Kohlstädt
Head of Press and Public Relations
German Cancer Research Center
Im Neuenheimer Feld 280
D-69120 Heidelberg
T: +49 6221 42 2843
F: +49 6221 42 2968
presse@dkfz.de
www.dkfz.de
Doris Rübsam-Brodkorb
Universitätsklinikum Heidelberg und Medizinische Fakultät der Universität Heidelberg
Presse- und Öffentlichkeitsarbeit
Im Neuenheimer Feld 672
69120 Heidelberg
Tel.: +49 6221 56-5052
Fax: +49 6221 56-4544
E-Mail: doris.ruebsam-brodkorb@med.uni-heidelberg.de
www.klinikum.uni-heidelberg.de
The National Center for Tumor Diseases (NCT) Heidelberg
The National Center for Tumor Diseases (NCT) Heidelberg is a joint institution of the German Cancer Research Center, Heidelberg University Hospital and German Cancer Aid. The NCT's goal is to link promising approaches from cancer research with patient care from diagnosis to treatment, aftercare and prevention. The interdisciplinary tumor outpatient clinic is the central element of the NCT. Here the patients benefit from an individual treatment plan prepared in a timely manner in interdisciplinary expert rounds, the so-called tumor boards. Participation in clinical studies provides access to innovative therapies. The NCT thereby acts as a pioneering platform that translates novel research results from the laboratory into clinical practice. The NCT cooperates with self-help groups and supports them in their work. Since 2015, a second site for the NCT beside Heidelberg has been under development in Dresden.
German Cancer Consortium (DKTK)
The German Cancer Consortium (DKTK) is a joint long-term initiative involving the German Federal Ministry of Education and Research (BMBF), participating German states and the German Cancer Research Center (DKFZ) and was established as one of six German Health Research Centres (DZGs).
As DKTK’s core center the DKFZ works together with research institutions and hospitals in Berlin, Dresden, Essen/Düsseldorf, Frankfurt/Mainz, Freiburg, Munich, Heidelberg and Tübingen to create the best possible conditions for clinically oriented cancer research. The consortium promotes interdisciplinary research at the interface between basic research and clinical research, as well as clinical trials for innovative treatments and diagnostic methods. Another key focus of the consortium’s work is on developing research platforms to speed up the application of personalized cancer treatments and to improve the diagnosis and prevention of cancer.
The German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ)
The German Cancer Research Center (DKFZ) with its more than 3,000 employees is the largest biomedical research institute in Germany. At DKFZ, more than 1,000 scientists investigate how cancer develops, identify cancer risk factors and endeavor to find new strategies to prevent people from getting cancer. They develop novel approaches to make tumor diagnosis more precise and treatment of cancer patients more successful. The staff of the Cancer Information Service (KID) offers information about the widespread disease of cancer for patients, their families, and the general public. Jointly with Heidelberg University Hospital, DKFZ has established the National Center for Tumor Diseases (NCT) Heidelberg, where promising approaches from cancer research are translated into the clinic. In the German Consortium for Translational Cancer Research (DKTK), one of six German Centers for Health Research, DKFZ maintains translational centers at seven university partnering sites. Combining excellent university hospitals with high-profile research at a Helmholtz Center is an important contribution to improving the chances of cancer patients. DKFZ is a member of the Helmholtz Association of National Research Centers, with ninety percent of its funding coming from the German Federal Ministry of Education and Research and the remaining ten percent from the State of Baden-Württemberg.
Heidelberg University Hospital and Medical Faculty Heidelberg
Health care, research and teaching of international standing
Heidelberg University Hospital is one of the most important medical centers in Germany; Heidelberg University's Medical Faculty is one of Europe's most prestigious biomedical research facilities. Their shared objective is the development of innovative diagnostics and treatments and their prompt implementation for the benefit of the patient. The hospital and faculty employ approximately 12 600 individuals and are involved in training and qualification. Every year approximately 66 000 patients are treated as inpatients or day patients in more than 50 specialized clinical departments with about 1 900 beds, with more than 1 million patients being treated as outpatients. The Heidelberg Curriculum Medicinale (HeiCuMed) is at the forefront of medical training in Germany. At present approx. 3500 prospective physicians are studying in Heidelberg.