Joint press release of KiTZ and NCT Heidelberg
Neuroblastoma can spread relentlessly or shrink spontaneously. Scientists from the Hopp Children’s Cancer Center Heidelberg (KiTZ), the German Cancer Research Center (DKFZ), the University of Heidelberg and the National Center for Tumor Diseases (NCT) Heidelberg have shown that some malignant neuroblastomas employ a trick to avoid cell death: they use a special mechanism to lengthen the telomeres at the end of their chromosomes. This makes them very different from other high-risk neuroblastomas and those with a favorable prognosis. The results may help to provide new therapy concepts tailored to this subgroup.
The Hopp Children’s Cancer Center Heidelberg (KiTZ) is a joint institution of the German Cancer Research Center (DKFZ), University Hospital Heidelberg (UKHD) and the University of Heidelberg (Uni HD).
The National Center for Tumor Diseases (NCT) Heidelberg is a joint institution of the German Cancer Research Center (DKFZ), University Hospital Heidelberg (UKHD) and the German Cancer Aid (DKH).
Neuroblastomas are the second most common form of solid tumor found in children, after brain tumors. The tumors develop from immature precursor cells of the nervous system and occur in the adrenal glands, or along the spine – in the neck, chest or abdomen. In some cases, neuroblastomas shrink and completely disappear without any therapy at all. But in around half of all patients, even highly intensive treatment is unable to prevent the tumor from growing.
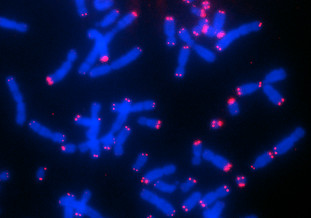
Malignant neuroblastoma cells employ a trick so that they can carry on dividing: they lengthen their telomeres, the caps at the end of their chromosomes. In healthy body cells, the telomeres are shortened with every cell division. Once a critical length is reached, telomer shrinkage leads to growth stoppage or cell death. By contrast, in stem cells and most cancer cells, the length of the telomeres is kept above the critical threshold by means of lengthening mechanisms, making the cells practically ‘immortal’.
“The cancer cells do this in one of two ways at the molecular level,” explains Sabine Hartlieb from the KiTZ, the DKFZ and the University of Heidelberg, who is one of the two lead authors of the paper. “They either overactivate the telomerase enzyme, which also keeps the telomere length as constant as possible during cell division in healthy stem cells, for instance. Or they lengthen the shortened chromosome ends by rearranging their telomere segments.” This latter mechanism is what scientists call the alternative lengthening of telomeres. “Tumors in which telomere lengthening is activated, by either of these methods, all have a poor prognosis,” says Frank Westermann, who was leading the study at the KiTZ and the DKFZ.
This is confirmed by the data from 760 neuroblastoma patients in the study. However, in nearly half of the patients who suffered a relapse, it was not overactivation of telomerase, but the alternative lengthening of telomeres that was responsible.
By integrating genetic and epigenetic data and the first ever analysis of all the proteins present in the tumor, the scientists investigated which molecular processes promote this specific lengthening mechanism. Summarizing the results, Lina Sieverling, one of the two lead authors, who works at the DKFZ and the NCT in Heidelberg, says, “Tumors with this telomere lengthening mechanism differ significantly from other neuroblastoma subgroups in terms of certain mutations, protein complexes and epigenetic signals.” For instance, the study found that malignant neuroblastoma have methylation signals on their protein histone 3 in the telomere region. This packages DNA into chromosomes, giving them a particularly compact and stable structure. Numerous other proteins from these tumors also showed characteristic modifications that were only partially visible, if it all, at genetic level. Scientists have long known that changes to the ATRX gene are associated with the alternative mechanism. Now they have been able to show that the ATRX/DAXX protein complex is modified in all tumors of this subgroup, even in cases where there was no discernible genetic mutation.
“These clear molecular differences are also reflected in the different clinical course of the disease in this group of patients,” stresses Frank Westermann. “Until now, all these young patients have been treated with the same chemotherapy protocols, which primarily attack fast-growing cancer cells. However, cancer cells with the alternative mechanism tend to grow slowly, but keep on growing, and are extremely resilient. We are dealing here with constantly recurring tumors, for which these standard therapies are very probably not the best solution,” says Westermann. “In the next stage, we will work on developing a specific therapy for these tumors because these children urgently need new treatment concepts. And such concepts could presumably also be used to treat other types of cancer that make use of the same special telomere lengthening mechanism.”
Original publication:
S. A. Hartlieb, L. Sieverling et al. Alternative lengthening of telomeres in childhood neuroblastoma from genome to proteome. In: Nature Communications (online publication 24th 2021). DOI: 10.1038/s41467-021-21247-8
An image for this press release is available for download at:
https://www.kitz-heidelberg.de/fileadmin/media/kitz/news/2021/Neuroblastom_CHLA90.jpg
Caption:
Human chromosomes of neuroblastoma cells. Chromosome ends (telomeres) are shown in red, which are particularly long here. Another characteristic of certain neuroblastoma cells is that the length of the telomeres differs from cell to cell.
Note on use of images related to press releases
Use is free of charge. The German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) permits one-time use in the context of reporting about the topic covered in the press release. Images have to be cited as follows: “Source: Larissa Savelyeva/KiTZ”.
Distribution of images to third parties is not permitted unless prior consent has been obtained from DKFZ’s Press Office (phone: +49 6221 42-2854, E-mail: presse@dkfz.de). Any commercial use is prohibited.
Press contact:
Dr. Alexandra Moosmann
Head of communications KiTZ
Hopp Children’s Cancer Center Heidelberg (KiTZ)
Im Neuenheimer Feld 130.3 / 7.320
D-69120 Heidelberg
T: +49 (0) 6221 56 36434
a.moosmann@kitz-heidelberg.de
presse@kitz-heidelberg.de
Dr. Sibylle Kohlstädt
Strategic Communication and Public Relations
German Cancer Research Center
Im Neuenheimer Feld 280
D-69120 Heidelberg
T: +49 6221 42 2843
F: +49 6221 42 2968
S.Kohlstaedt@dkfz.de
presse@dkfz.de
Doris Rübsam-Brodkorb
Corporate Communications Heidelberg University Hospital and Medical Faculty
Im Neuenheimer Feld 672
D-69120 Heidelberg
T: +49 6221 56-5052
F: +49 6221 56-4544
doris.ruebsam-brodkorb@med.uni-heidelberg.de
Dr. Friederike Fellenberg
National Center for Tumor Diseases Heidelberg (NCT)
Press and Public Relations
Im Neuenheimer Feld 460
69120 Heidelberg
Tel.: +49 6221 56-5930
Fax: +49 6221 56-5350
Email: friederike.fellenberg@nct-heidelberg.de
www.nct-heidelberg.de
The Hopp Children's Cancer Center Heidelberg (KiTZ)
The „Hopp Children's Cancer Center Heidelberg” (KiTZ) is a joint institution of the German Cancer Research Center (DKFZ), Heidelberg University Hospital and Heidelberg University. As the National Center for Tumor Diseases (NCT), which focusses on adult oncology, the KiTZ is based on the US model of so-called “Comprehensive Cancer Centers” (CCC). As a therapy and research center for oncologic and hematologic diseases in children and adolescents, the KiTZ is committed to scientifically exploring the biology of childhood cancer and to closely linking promising research approaches with patient care– from diagnosis to treatment and aftercare. Children suffering from cancer, especially those with no established therapy options, are given an individual therapy plan in the KiTZ, which is created by interdisciplinary expert groups in so-called tumor boards. Many young patients can participate in clinical trials which ensures access to new therapy options. Thus, the KiTZ is a pioneering institution for transferring research knowledge from the laboratory to the clinic.
While the KiTZ focuses on pediatric oncology, the focus of the National Center for Tumor Diseases (NCT), founded in 2004, is adult oncology. Both facilities in Heidelberg are based on the US model of so-called "Comprehensive Cancer Centers" (CCC).
The German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ)
The German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) with its more than 3,000 employees is the largest biomedical research institution in Germany. At DKFZ, more than 1,300 scientists investigate how cancer develops, identify cancer risk factors and endeavor to find new strategies to prevent people from getting cancer. They develop novel approaches to make tumor diagnosis more precise and treatment of cancer patients more successful.
DKFZ’s Cancer Information Service (KID) provides individual answers to all questions about cancer for patients, the general public, and health care professionals.
Jointly with partners from Heidelberg University Hospital, DKFZ runs the National Center for Tumor Diseases (NCT) located in Heidelberg and Dresden, and, also in Heidelberg, the Hopp Children’s Cancer Center (KiTZ). In the German Cancer Consortium (DKTK), one of six German Centers for Health Research, DKFZ maintains translational centers at seven university partnering sites. Combining excellent university hospitals with high-profile research at a Helmholtz Center at the NCT and DKTK sites is an important contribution to the endeavor of translating promising approaches from cancer research into the clinic in order to improve the chances of cancer patients.
DKFZ is a member of the Helmholtz Association of National Research Centers, with ninety percent of its funding coming from the German Federal Ministry of Education and Research and the remaining ten percent from the State of Baden-Württemberg.
Heidelberg University Hospital and Medical Faculty
Internationally recognized patient care, research, and teaching
Heidelberg University Hospital is one of the largest and most prestigious medical centers in Germany. The Medical Faculty of Heidelberg University belongs to the internationally most renowned biomedical research institutions in Europe. Both institutions have the common goal of developing new therapies and implementing them rapidly for patients. With about 13,000 employees, training and qualification is an important issue. Every year, around 65,000 patients are treated on an inpatient basis, 56,000 cases on a day patient basis and more than 1,000,000 cases on an outpatient basis in more than 50 clinics and departments with almost 2,000 beds. Jointly with the German Cancer Research Center (DKFZ) and German Cancer Aid, Heidelberg University Hospital has established the National Center for Tumor Diseases (NCT) Heidelberg, where promising approaches from cancer research are translated into the clinic. Currently, about 3,700 future physicians are studying in Heidelberg; the reform Heidelberg Curriculum Medicinale (HeiCuMed) is one of the top medical training programs in Germany.
National Center for Tumor Diseases Heidelberg (NCT)
The National Center for Tumor Diseases (NCT) Heidelberg is a joint institution of the German Cancer Research Center, Heidelberg University Hospital (UKHD) and German Cancer Aid. The NCT's goal is to link promising approaches from cancer research with patient care from diagnosis to treatment, aftercare and prevention. This is true for diagnosis and treatment, follow-up care or prevention. The interdisciplinary tumor outpatient clinic is the central element of the NCT. Here, the patients benefit from an individual treatment plan prepared in interdisciplinary expert rounds, so-called tumor boards. Participation in clinical studies provides access to innovative therapies. The NCT thereby acts as a pioneering platform that translates novel research results from the laboratory into clinical practice. The NCT cooperates with self-help groups and supports them in their work. Since 2015, the NCT Heidelberg has maintained a partner site in Dresden. The Hopp Children's Cancer Center (KiTZ) was established in Heidelberg in 2017. The pediatric oncologists at KiTZ work together in parallel structures with the NCT Heidelberg.