Head and neck tumours: improving the tolerability of radiotherapy
Side effects can occur during and after irradiation in the head and neck region, in particular painful inflammation of the oral mucosa. Ideally, if possible, only the malignant tumor should be irradiated and not the adjacent healthy tissue, which is only partially successful despite state-of-the-art irradiation techniques. Conventionally, a dental splint is used for radiotherapy of head and neck tumors, which lowers the dose to the directly adjacent mucosa. Scientists from the Department of Radiation Oncology and Radiotherapy, the Department of Oral and Maxillofacial Surgery and the Department of Otolaryngology at the NCT Heidelberg and UKHD now want to improve the tolerability of head and neck irradiation as part of a collaborative project.
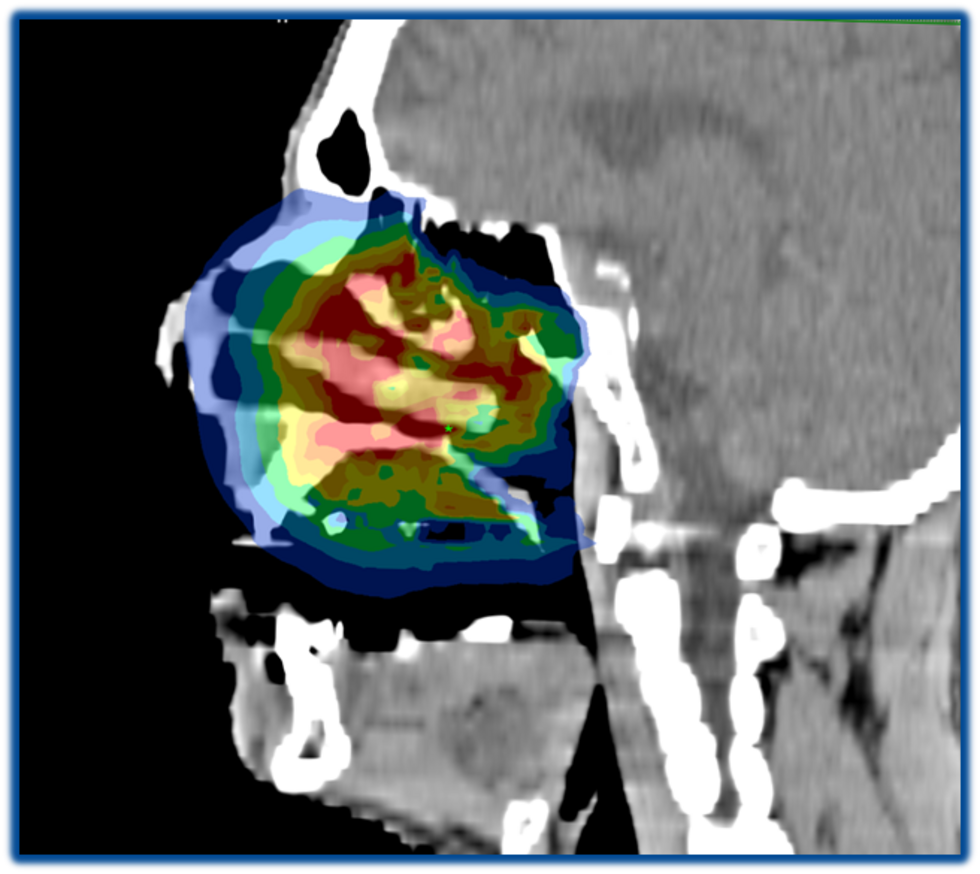
Using 3D printer-based and subsequently customized tissue retractors, large parts of the mucosa can be relocated from the high-dose area of irradiation, which brings significant advantages for patients. For example, in the case of a tumor in the upper jaw, the tongue is pushed down and thus not "co-irradiated" unintentionally with a high dose. This is expected to result in fewer side effects such as dry mouth, difficulty swallowing and weight loss, as well as associated stays in hospital. This promising approach is now to be investigated in a clinical trial with the aim of reducing the side effect rate and improving patients' quality of life.
Head and neck tumors: help for stressful therapy situation
Therapy varies depending on the type and location of the head and neck tumor. In most cases, irradiation is required, but this is carried out under particularly stressful conditions for the patient, for example by making a plastic mask for the head or keeping the patient in a fixed position during treatment. A considerable proportion of patients therefore experience anxiety and panic attacks, which in turn can lead to increased use of sedatives and therapy discontinuation.
Psycho-oncological and online interventions can help patients in the very stressful therapy situation. With the help of exercises from trauma therapy, the patients' self-soothing skills should be trained.
In a feasibility study in cooperation with the Psychooncology Section and the Department of Radiation Oncology, physicians and scientists were able to show that there is a high demand for supportive psychooncological services to accompany the stressful treatments. In a clinical study, physicians Imad Maatouk and Sebastian Adeberg from the NCT Heidelberg and UKHD now want to examine the extent to which such services can demonstrably help patients. In addition to face-to-face appointments where patients are taught self-soothing strategies, they are given access to an online support service. This web-based program provides information on radiation and exercises to help patients cope better with the difficult treatment situation.
Melanoma: Can the therapeutic success of immunotherapy be predicted?
Immuno-oncological approaches, such as treatment with so-called checkpoint inhibitors, have significantly improved the survival of patients with metastatic melanoma. However, less than half of the patients benefit permanently from the therapy and until today researchers know little about what really accounts for this therapy resistance.
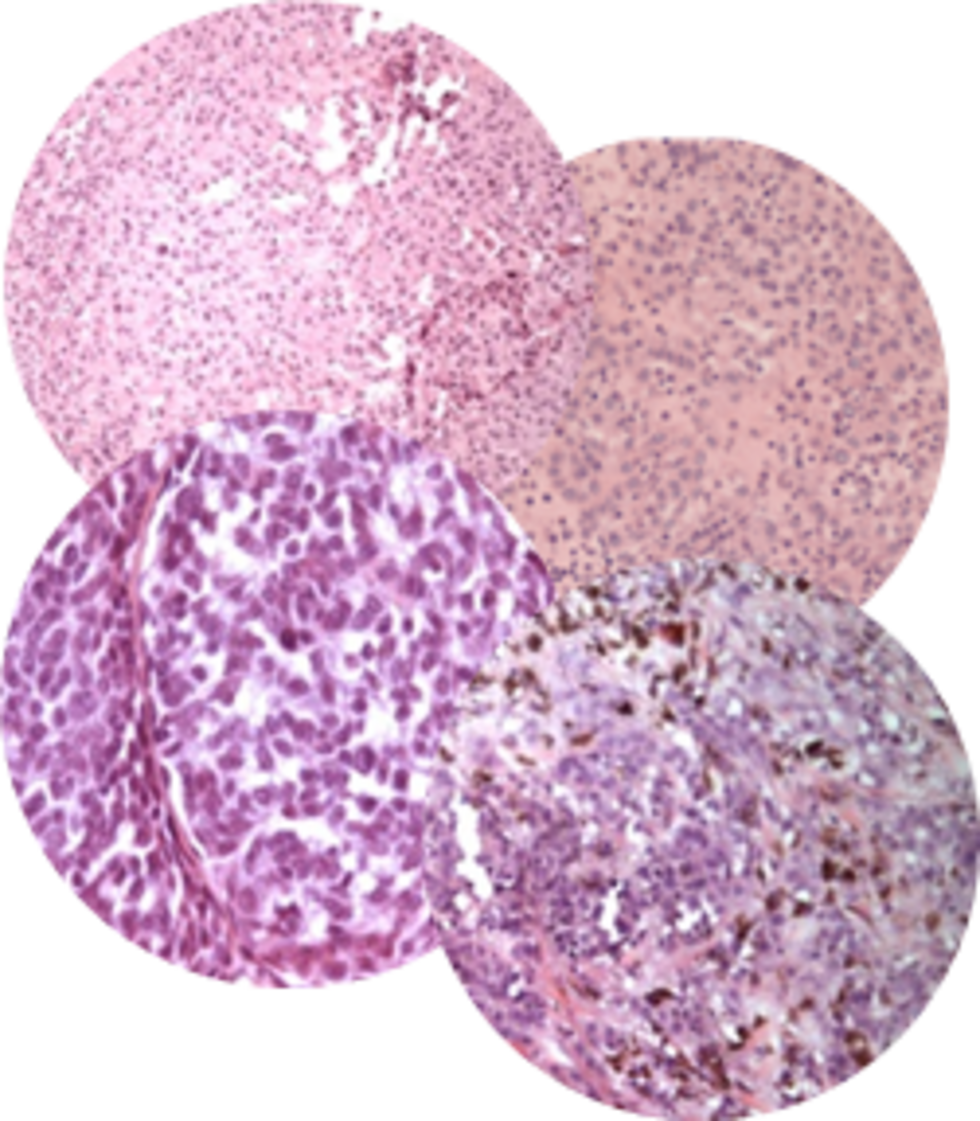
Studies show that the presence of immune cells in tumor tissue in particular, but also the amount of a specific protein called PD-L1, correlates with the response of immunotherapy directed against PD1.
A closer look at the cell structure of a melanoma and its metastases shows that these can look very different from patient to patient. With the help of artificial intelligence (AI), NCT Heidelberg physicians and scientists Jessica Hassel and Jakob Kather want to find these differences using an adaptive computer-based algorithm. With the help of AI, the researchers hope to be able to predict before the start of immunotherapy whether it will be effective or whether the patient can be spared the treatment and any side effects.
Facilitated search for oncology studies in Germany
Participation in clinical trials gives patients access to innovative therapies. In Germany, there are currently around 800 trials available for cancer. Slightly less than five percent of adult cancer patients are currently treated in such studies. One reason for the rather low participation rate is the fact that it is difficult for doctors, but also for patients, to find out about suitable studies.
The most important websites to find suitable studies for patients are CLINICALTRIALS.GOV and CLINICALTRIALSREGISTER.EU. Since important information, for example, on diagnoses, therapeutic procedures and molecular criteria, which are becoming increasingly important in modern oncology, is often incomplete or contained in a form that is difficult to find, a search is often very time-consuming. Nevertheless, it is not uncommon for interesting study offers not to be found.
The scientists and physicians Simon Kreutzfeldt and Daniel Hübschmann from the NCT Heidelberg now want to create a central platform that will make it easier for physicians and patients to search for suitable studies for cancer diseases in Germany. The study data from the two registries CLINICALTRAILS.GOV and CLINICALTRIALSREGISTER.EU will be continuously fed into this database in an automated way. Additional data are added manually to each study, so that even detailed searches can be implemented quickly and produce largely complete hit lists. The accurate recording of molecular criteria will facilitate the use especially for precision oncology therapies and allow an automated integration into molecular tumor boards. Finally, a German-language user interface and German short descriptions of studies will also provide patients themselves with a useful source of information.
Specific training for patients with bone metastases
Many patients with advanced cancer suffer from bone metastases. In addition to pain, the metastases also cause bone fractures even when little force is applied. Affected patients therefore usually hardly dare to engage in sporting activities. However, this in turn increases the risk of bone fractures, as the supporting muscles are broken down and patients fall more quickly. Overall, performance deteriorates and with it the quality of life. So far, it has not been investigated in which situations exactly these bone fractures occur. A survey of those affected is now to record and analyze the circumstances of the fractures and the localization of the bone metastasis.

Based on the results, the sports scientists from the Department of Medical Oncology at the NCT Heidelberg, Friederike Rosenberger and Joachim Wiskemann, together with their medical colleagues from the Clinic for Orthopedics and Trauma Surgery at the UKHD, Burkhard Lehner and Georg Omlor, want to develop specific training units for these patients. An educational flyer with preventive exercise offers combined with strength exercises will then provide information in a compact form and help to be physically active safely despite bone metastases.
Virtual Reality: A trip out of the hospital room
In the course of immunotherapy prior to stem cell transplantation or during prolonged chemotherapy, it is very stressful for patients to be cut off from the outside world for weeks at a time. With 360-degree images, VR goggles offer the opportunity to enter another world for a certain period of time.
Diving into the virtual world can help the patient to be distracted from his treatment and the situation for a short time. Self-awareness is strengthened and, in combination with pain medication, a positive effect on pain behavior can be achieved. The new VR glasses can also be used for guided breathing and relaxation exercises.
The nursing team at the Clinic for Hematology, Oncology and Rheumatology and the NCT ward at the UKHD would like to help patients achieve a better quality of life during their hospital stay by providing different perspectives.







