Novel immunotherapy for advanced melanoma of the eye
Press release from Heidelberg University Hospital (UKHD)
A new immunotherapy couples immune cells directly to tumor cells. This enables the immune cells to specifically destroy the cancer cells, which can improve the survival time of patients with melanoma of the eye. The scientists from Heidelberg and Paris have published the results of their study in the New England Journal of Medicine.
There are now very effective immunotherapies for patients with malignant melanoma. Rarely, however, melanoma can also occur within the eye. These tumors often spread rapidly and are incurable. A recently approved T-cell engager, Tebentafusp, represents a new therapeutic option. It can extend survival time by several months. This was the result of an international multicenter Phase III study led by Professor Jessica Hassel, Heidelberg University Hospital (UKHD), National Center for Tumor Diseases (NCT) Heidelberg and Heidelberg Medical Faculty of Heidelberg University, and Dr. Sophie Piperno-Neumann from the Institut Curie in Paris, which has now been published in the "New England Journal of Medicine". Tebentafusp belongs to the class of immunotherapeutics. It simultaneously binds to both the tumor cells and certain immune cells (T lymphocytes) and thus generates an immune response against the cancer. The study involved 378 patients in whom the melanoma had already metastasized. The current publication focuses on the survival rates three years after the start of treatment.
One-year survival rate significantly improved
Melanomas of the eye develop in the choroid (uvea) of the eye, in the iris and in the structures to which the lens is attached. Every year in Germany, around 400 to 500 predominantly older people between the ages of 60 and 70 are diagnosed with this most common type of eye tumor in adults. There are various treatment options, ranging from laser therapy and radiation to removal of the eye. However, around half of those affected succumb to the numerous metastases that uveal melanoma forms within a short period of time, often within the first year of diagnosis.
The new T cell activator, the "T cell engager" Tebentafusp, has significantly improved the one-year survival rate: "In our study, more than 70 percent of patients survived the first year, with manageable side effects such as chills, fever and rash, especially at the start of treatment," explains Professor Jessica Hassel, Head of the Dermatooncology Section at UKHD and NCT Heidelberg. "As the data now published show for the first time, this survival advantage continues up to three years after diagnosis." More than a quarter (27 percent) of patients who received Tebentafusp were still alive after three years. Among participants in the control group, who received one of the established standard therapies with other antibodies, the figure was 18 percent. Allocation to the Tebentafusp or control group was randomized at the start of therapy.
Bispecific for tumor and immune cells
T-cell engagers are bispecific constructs: On the one hand, they bind to small protein fragments on the tumor cell surface and, on the other, to a structure on the surface of those immune cells (T lymphocytes) that can destroy these cancer cells. The effect surpasses all previously used therapies for disseminated uveal melanoma.
Although the disease can only be permanently controlled in a small number of patients over the course of three years with Tebentafusp, the experts still rate the results as extremely positive: "With previous therapies, the survival prognosis for patients with metastatic uveal melanoma was extremely poor. The results show us that we are on the right track with the T-cell engagers to improve the prognosis even for patients with difficult-to-treat cancers," says Jessica Hassel.
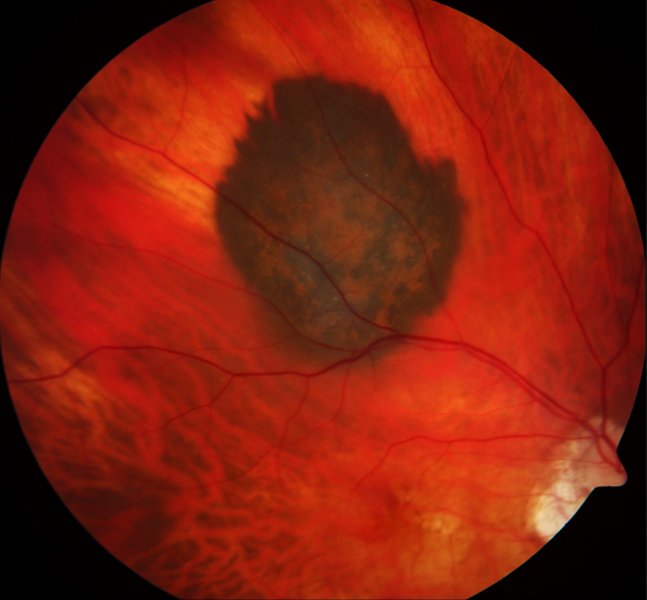
Image description
The choroidal melanoma stands out darkly against the healthy tissue at the back of the eye. The image is available for download here. Use of the image is free of charge, use is only permitted in connection with reporting on the topic of this press release. Use for commercial purposes is prohibited.
Literature
Hassel JC, Piperno-Neumann S, Rutkowski P, et al. Three-Year Overall Survival with Tebentafusp in Metastatic Uveal Melanoma. N Engl J Med. Published online October 21, 2023. doi:10.1056/NEJMoa2304753
Further information on the Internet
Hauttumorzentrum an UKHD und NCT Heidelberg
Contact
Prof. Dr. med. Jessica C. Hassel
Head of the Dermatooncology Section at the Department of Dermatology at Heidelberg University Hospital and the National Center for Tumor Diseases (NCT) Heidelberg
Medical Faculty Heidelberg of the University of Heidelberg
E-Mail: jessica.hassel(at)med.uni-heidelberg.de
You can also find this press release online in our UKHD Newsroom.
Heidelberg University Hospital and Faculty of Medicine: Internationally Renowned Patient Care, Research and Teaching
Heidelberg University Hospital (Universitätsklinikum Heidelberg, UKHD) is one of the largest and most prestigious medical centers in Germany. The Medical Faculty of Heidelberg University (Medizinische Fakultät Heidelberg, MFHD) belongs to the internationally renowned biomedical research institutions in Europe. Both institutions have the common goal of developing new therapies and implementing them rapidly for patients. Heidelberg University Hospital and the Medical Faculty of Heidelberg University employs around 14.500 employees and is committed to providing trainings and qualifications. Every year, around 86,000 patients and more than 1.100.000 outpatient cases are treated in more than 50 clinical departments with almost 2.500 beds.
Together with the German Cancer Research Center (Deutsches Krebsforschungszentrum, DKFZ) and the German Cancer Aid, the UKHD established the first National Center for Tumor Diseases (NCT) in Heidelberg. The goal is to provide care at the highest level as an oncology center of excellence and to rapidly transfer promising approaches from cancer research to the hospital. In addition, the UKHD operates in partnership with the DKFZ and the University of Heidelberg the Hopp Children’s Cancer center Heidelberg (KiTZ), a unique and nationally known therapy and research center for oncological and hematological diseases in children and adolescents.
The Heidelberg Curriculum Medicinale (HeiCuMed) is one of the top medical training programs in Germany. Currently, there are about 4.000 future physicians studying in Heidelberg.
Dr. Stefanie Seltmann
Press Officer
Head of Corporate Communications
Phone +49 6221 56-5052
Stefanie.Seltmann(at)med.uni-heidelberg.de
Julia Bird
Deputy Press Officer
Phone +49 6221 56-7071
Fax +49 6221 56-4544
julia.bird(at)med.uni-heidelberg.de







